This article describes Boerhaave syndrome, including its symptoms, causes, and treatment.

Boerhaave syndrome is very rare. It gets its name from
Most esophageal ruptures are the result of endoscopic procedures. In Boerhaave syndrome, the rupture is not related to any kind of medical intervention.
The rupture most often occurs in the lower part of the esophagus, near the stomach.
Other names for this condition include spontaneous esophageal rupture and effort rupture of the esophagus. Perforation and holes in the esophagus also describe a rupture.
The classic symptoms of Boerhaave syndrome are called the Mackler triad. The triad consists of chest pain, vomiting, and subcutaneous emphysema. This last symptom is basically air trapped in the tissues under the skin.
While the triad is the classic presentation, most people do not have all three symptoms. Subcutaneous emphysema is present about 30% of the time. This can make Boerhaave syndrome hard to diagnose.
Other possible symptoms include:
- abdominal pain
- difficulty swallowing or speaking
- fast heart rate and breathing
- fever
- neck or shoulder pain
- shortness of breath
These symptoms are very similar to other emergent conditions, such as heart attack and pulmonary embolism. This adds to the difficulty of diagnosing Boerhaave syndrome. It is common to mistake it for these other conditions because it is so rare.
Boerhaave syndrome occurs when pressure inside the esophagus
In most cases, the rupture occurs during vomiting when the upper esophageal sphincter does not relax. Normally, this muscle remains contracted to tightly seal the top of the esophagus. Nerve signals tell it to relax when you swallow food or vomit.
In Boerhaave syndrome, the upper esophageal sphincter does not relax, causing a massive increase in pressure. This leads to the rupture and perforation of the esophagus.
The main risk factor for Boerhaave syndrome is heavy alcohol consumption. Usually, this is in combination with eating large amounts of food. The condition most commonly affects biological males and peaks between the ages of 50 and 70 years old.
Other causes may include:
- defecating
- giving birth
- having a seizure
- retching
- sustaining trauma to the abdomen
- weightlifting
All of these can cause the kind of rise in pressure that can rupture the esophagus.
Diagnosing Boerhaave syndrome can be
However, lab tests are not helpful for diagnosing an esophageal rupture. Instead, doctors rely on imaging exams, including:
- chest X-ray, which can still be normal in about 15% of people with a rupture
- esophagogram, or a barium swallow
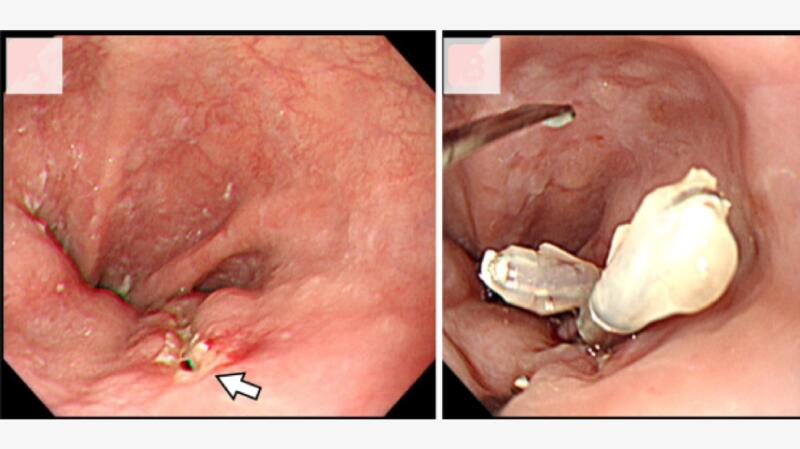
The esophagogram is the main tool for diagnosing Boerhaave syndrome. However, doctors use a water-soluble contrast instead of barium. This reduces irritation if the contrast leaks out of the hole in the esophagus.
Some doctors use CT scans instead of an esophagogram. Most doctors do not use endoscopy, as it can worsen the perforation.
Boerhaave syndrome is a surgical emergency. When doctors find the rupture within the first 24 hours, surgical repair of the esophagus is the
When a diagnosis occurs after 24 hours, the tissue around the rupture is either too swollen, crumbly, or stiff to surgically repair. It is often necessary to remove the esophagus instead of repairing it. Doctors can then perform an esophageal replacement after 6 weeks.
Boerhaave syndrome is very rare. Excessive alcohol consumption is the main risk factor for developing it. Therefore, the main way to prevent it is by limiting alcohol consumption.
You can also seek help for alcohol misuse and alcohol use disorder.
Boerhaave syndrome has a
People who have surgery to repair the esophagus within 24 hours have a good outlook. The survival rate for these patients is about 75%.
Delayed diagnosis and treatment leads to poor outcomes. The overall mortality rate is approximately 40%.
Other complications can include:
- acute respiratory distress syndrome, in which fluid leaks into the lungs
- empyema, in which pus collects between the lungs and the lining of the chest cavity
- mediastinitis, in which the chest cavity between the lungs swells
- pleural effusion, in which fluid builds up around the lungs
- pneumomediastinum, in which air is present in the chest cavity between the lungs
Mallory-Weiss syndrome is a tear in the lining of the esophagus. It does not go all the way through the esophagus wall. The tear can result in bleeding that ranges from mild to severe.
Like Boerhaave syndrome, episodes of powerful vomiting are the
Unlike Boerhaave syndrome, Mallory-Weiss syndrome is rarely fatal. Most cases resolve without treatment, as the bleeding stops on its own. Only 10% of cases result in severe bleeding.
Boerhaave syndrome is a life threatening emergency. It occurs when increased pressure in the esophagus causes a rupture. In most cases, the cause is forceful vomiting.
Symptoms can include chest pain and other problems that mimic several other medical conditions. This plus the rarity of the syndrome make diagnosing it challenging.
When a diagnosis occurs within 24 hours, surgical treatment often has a good outcome. However, the syndrome has a high mortality rate, especially with delayed diagnosis.